Texas Biomed researchers find promising benefits for gut health, serotonin levels and more. The study, reported in Science Advances, could have broad implications for other diseases linked to gut inflammation.
SAN ANTONIO (Nov. 6, 2025) – Long-term, low doses of THC mitigate many harmful side effects and inflammation caused by HIV and antiretroviral therapy (ART), according to new research from Texas Biomedical Research Institute.
THC is short for tetrahydrocannabinol, the main active compound in cannabis. The preclinical study used very low doses of THC, meaning the compounds don’t trigger overt nervous system effects such as euphoria, or a “high.”
The benefits included increased production of the chemical serotonin, while inflammation, cholesterol and harmful secondary bile acids were all reduced. Notably, levels of ART drugs, which can be toxic to the liver over time, were lower in blood plasma without affecting viral suppression. The detailed findings, made in animal models representing people with HIV on ART, were recently published in Science Advances.
Managing side effects

ART does a very good job at suppressing HIV to undetectable levels. Once a death sentence, HIV is now a manageable disease. But as people live longer with HIV, they are experiencing substantial side effects from the virus and the medications.
“People living with HIV experience chronic inflammation, which leads to many co-morbidities such as cardiovascular disease, liver disease and some neurological diseases,” said Professor Mahesh Mohan, DVM, Ph.D. “Our lab is interested in finding solutions to help address this.”
The current study builds on previous research in Dr. Mohan’s lab into therapeutic uses of low-dose THC – similar to FDA-approved THC medications for treating chemotherapy-induced nausea and vomiting, and AIDS-related anorexia and weight loss.
“No downsides”
Over the past three years, Lakmini Premadasa, Ph.D., a Staff Scientist in Dr. Mohan’s lab, analyzed hundreds of metabolites – small molecules that help carry out daily functions – to determine if this low-dose treatment given daily alongside ART benefited other parts of the body.
“There were no downsides,” Dr. Premadasa said. “I kept looking because I couldn’t believe it could all be good, but I really could not find any negative impacts.”
Lower ART-associated toxicity

For the study, two groups of rhesus macaques with simian immunodeficiency virus (SIV), the equivalent of HIV, were given ART for five months. One group also received low-dose THC, while the second group received a placebo. At five months, both groups had suppressed SIV to undetectable levels, but that is where the similarities stopped.
Notably, even though viral suppression was maintained, there were much lower levels of ART drugs circulating in the blood of the THC-treated group, compared to the group that only received ART.
“This was unexpected,” Dr. Premadasa said. “This suggests that THC is helping to metabolize the antiretroviral drugs faster, which is actually much better to protect the liver from toxicity associated with some currently prescribed ART drugs.”
Low-dose THC for a happy gut
Another key finding: serotonin, an important neurotransmitter that regulates mood along with a host of other functions, including sleep and digestion, was much higher in the THC-treated group compared to controls.
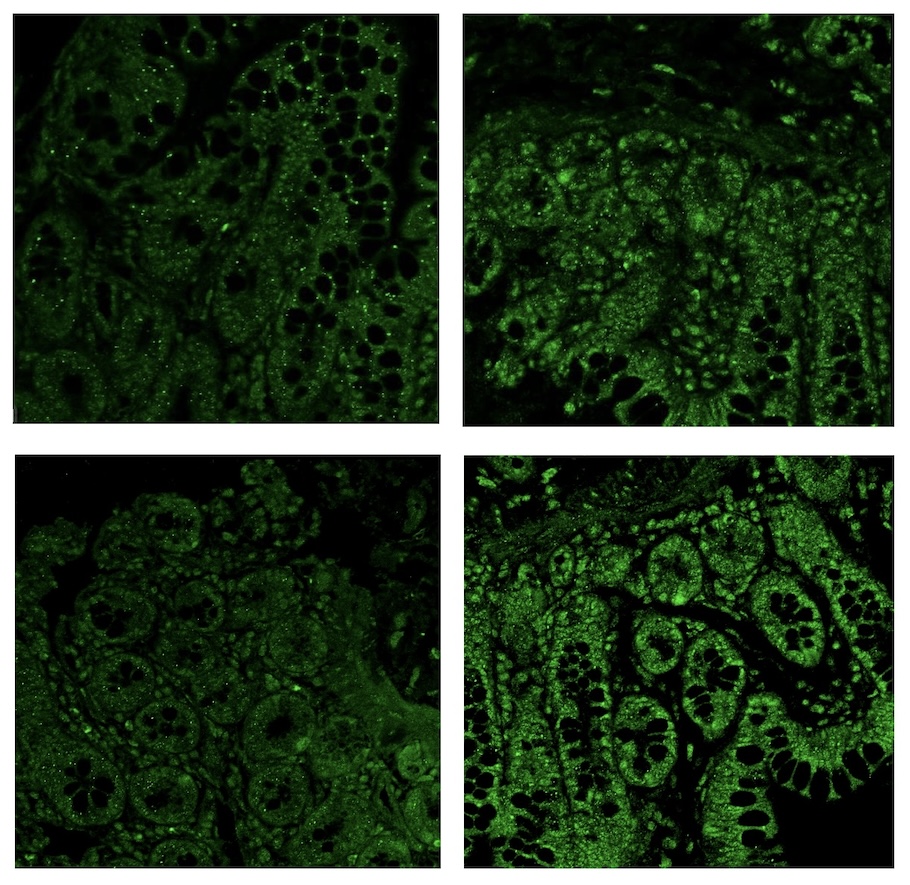
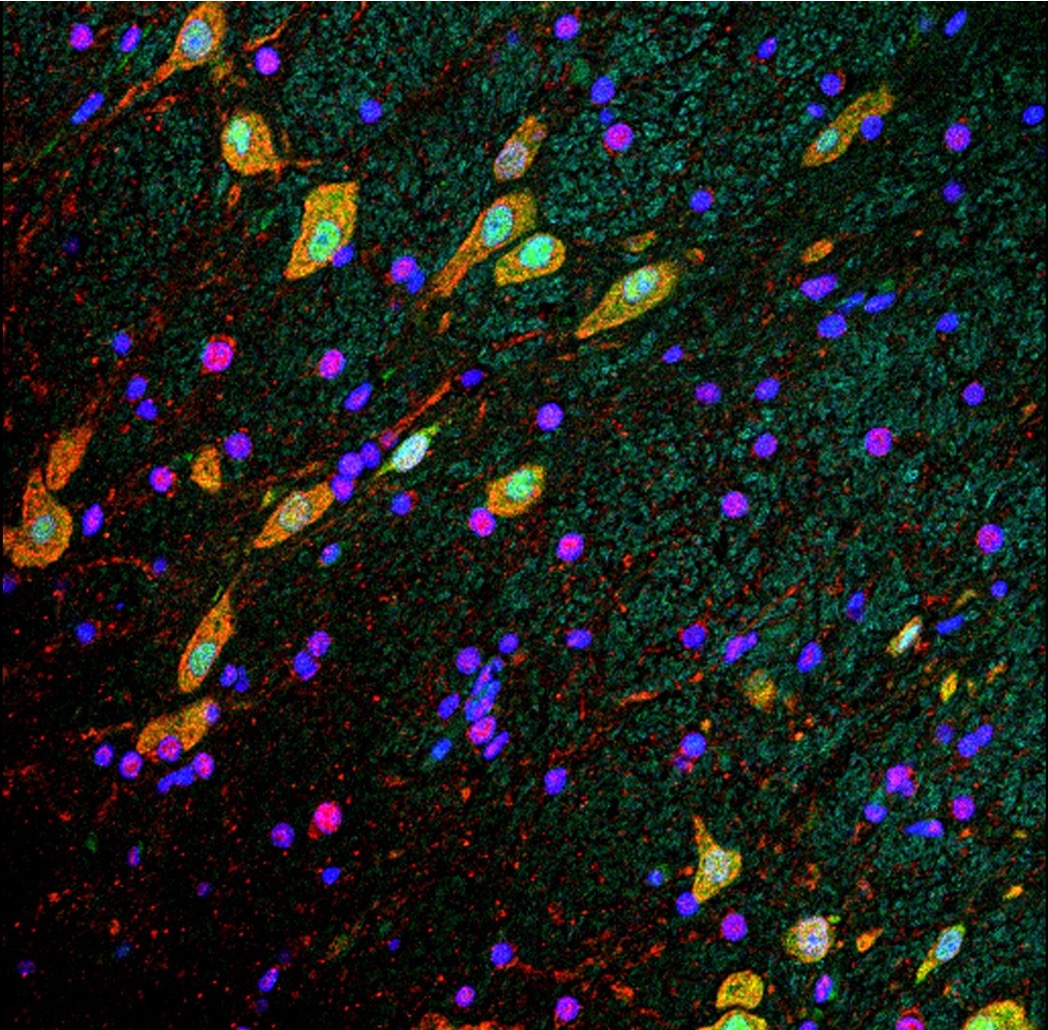
The increases were observed across multiple facets of serotonin production, which occurs primarily in the gut. Specifically, Dr. Premadasa found higher numbers of specialized enterochromaffin cells that produce serotonin and more good gut bacteria (L. plantarum) that facilitate serotonin production in the THC-treated group, compared to the control group. She also observed significant upregulation of serotonin receptors in the THC-treated group, which are required to convey signals from the gut to the brain via the vagus nerve, enhancing the gut-brain axis communication.
“This is an exciting finding that could be investigated further to address a range of conditions related to low serotonin levels, including depression, memory loss, brain fog and perhaps long-COVID symptoms,” Dr. Mohan said. “Reduced serotonin levels are known to disrupt signaling between the gut and brain, so improving those serotonin levels and communication with low-dose cannabinoids could offer a new or complementary treatment approach.”
More unexpected benefits
The THC-treated group also had a healthier, more balanced gut microbiome with higher levels of good gut bacteria, including species that help lower cholesterol. There were lower levels of secondary bile acids, which are toxic at high levels and can lead to blockage in the liver bile ducts (cholestasis), inflammation and scarring (cirrhosis) and end-stage liver disease.
Other metabolites were increased that help break down fatty acids, which helps reduce plaque that clogs arteries, thus improving cardiovascular health. In fact, levels of plaque-causing fatty acids, called long-chain acetylcholines, had returned to pre-infection levels in the THC-treated group, while the control group continued to have significantly elevated levels of harmful fatty acids.
Next steps
Since this work was completed in nonhuman primates, additional research is required to confirm if the same results occur in people. The results could also have implications for many other diseases linked to gut inflammation, such as irritable bowel syndrome, chronic liver disease and neurodegenerative diseases such as Alzheimer’s and Parkinson’s diseases.
The research team is now investigating the nonpsychoactive cannabidiol, or CBD, when it is combined with THC taken orally or in a shot alongside ART. The team also plans to research other minor cannabinoids and the aromatic compounds that give many plants their scents and flavors, called terpenes, in the future, as there is growing clinical interest in these compounds. The researchers caution that readers should not assume commercially available cannabinoid products offer the same benefits observed in this study because of the way different products are consumed and metabolized in the body. The best course of action is to consult with your healthcare provider before attempting any cannabinoid-based medications.
Paper:
Lakmini S. Premadasa et al., Supplementing HIV-ART with cannabinoids increases serotonin, BHB, and Ahr signaling while reducing secondary bile acids and acylcholines. Sci. Adv. 11, eadw4021(2025). DOI:10.1126/sciadv.adw4021
Funding:
National Institutes of Health award numbers R01DA042524 (M.M.) and R01DA052845 (M.M.), P30AI161943, P51OD011104 and P51OD111033.
Additional information:
Clinical trials evaluating the effects of THC and CBD in people living with HIV are being carried out and reported by other teams, including:
- UCSD – Cannabis Use, Cognition, and the Endocannabinoid System in HIV
- UCSD – Effects of Cannabidiol and Tetrahydrocannabinol on Microbiome and Neuroinflammation in HIV
- UCSD – Cannabis Effects on Antiretroviral Therapy Pharmacokinetics and Neurotoxicity
- McGill University & Université de Montréal – Effects of Oral Cannabinoids on Systemic Inflammation and Viral Reservoir Markers in People with HIV on Antiretroviral Therapy: Results of the CTN PT028 Pilot Clinical Trial
About Texas Biomed:
Texas Biomed is a nonprofit research institute dedicated to protecting the global community from infectious diseases. Through basic research, preclinical testing and innovative partnerships, we accelerate diagnostics, therapies and vaccines for the world’s deadliest pathogens. Our San Antonio campus hosts high containment laboratories and the Southwest National Primate Research Center. Our scientists collaborate with industry and researchers globally and have helped deliver the first COVID-19 vaccine, the first Ebola treatment and first Hepatitis C therapy. For more information, please visit https://txbiomed.org.