Researchers at Texas Biomed are advancing bird flu vaccine candidates and identifying potential treatment targets with mini 3D models of human airways.
Bird flu vaccine candidate highly effective in early studies
Researchers at Texas Biomedical Research Institute have developed a new, proof-of-concept vaccine to protect people from the bird flu strain currently circulating in the United States. The team, led by Professor Luis Martinez-Sobrido, Ph.D. and Staff Scientist Ahmed M. Elsayed, Ph.D., recently published initial results in npj Vaccines.
The live attenuated vaccine contains a weakened, or attenuated, version of the avian influenza virus that has sickened poultry and dairy cows throughout the U.S. since March 2024. The vaccine candidate showed high efficacy in cells and animal models. A single dose was enough to protect mice from highly pathogenic H5N1, which would otherwise be lethal.
The team is now working to develop versions of the vaccine that would address other bird flu strains circulating in hot spots around the world. Highly pathogenic avian influenza is naturally carried by migratory birds and waterfowl, but is deadly in domesticated chickens and turkeys.
“The ultimate aim is to develop a vaccine that could protect against multiple strains of bird flu, or even offer universal protection,” Dr. Elsayed said.
H5N1 has spread to a wide range of mammal species, from sea lions to cats and now dairy cattle. The current outbreak has sickened more than 70 people in the U.S. and killed at least one person to date, primarily through contact with infected livestock. Many experts are concerned the virus could evolve to spread between people, causing a more severe pandemic. The U.S. has emergency stockpiles of bird flu vaccines available, which are based on inactivated, or killed, versions of older bird flu viruses.
“Those vaccines have shown to work against the current strain of H5N1,” Dr. Martinez-Sobrido said. “However, live attenuated vaccines can offer longer-lasting and more robust protection.”
This research was funded through a pilot grant provided to Dr. Elsayed by the Texas Biomedical Forum, a philanthropic women’s organization dedicated to supporting Texas Biomed.
Organoids show how bird flu affects airway cells, reveal potential treatment target
The current strain of H5N1 bird flu circulating in the U.S. remodels the cells lining the human airway, causing scar tissue to form, researchers at Texas Biomed report in Emerging Microbes & Infections. Dr. Martinez-Sobrido and his team, led by Staff Scientist Hussin Rothan, Ph.D., identified a potential treatment target to reduce harmful inflammation associated with influenza infection.
The researchers used human airway organoids for this project. Organoids are miniature 3D models of specific tissues and have been developed in labs around the world for decades. These human airway organoids contain four critical cell types found in the trachea and they mimic the physical structure of the airway lining, or epithelium.
“They create mucus and you can see the cilia moving under the microscope,” said Dr. Rothan. “We can get much more detailed insight into tissue responses from these organoids than we can from single cell lines.”
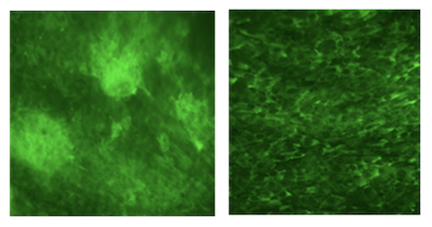
When exposed to a version of the bird flu first detected in Texas dairy cattle last spring, the organoids showed significant inflammatory responses, including increased production of cytokine proteins, and the development of fibrotic, or scar, tissue. The inflammatory response was far more severe for H5N1 compared to infection with a seasonal swine flu strain, H1N1.
The team found that briefly inhibiting a key driver of inflammation, known as the ROCK pathway, helped reduce the scarring. Specifically, they found that inhibiting the enzyme ROCK1 was more effective than inhibiting another enzyme, ROCK2.
“This was surprising because people usually focus on ROCK2,” Dr. Rothan said. “We now need to drill down and find out more about these interactions so we can find the most effective way to limit inflammation, not only for bird flu, but other respiratory viruses that affect the airway and lungs like SARS-CoV-2.”
Videos:
A human airway organoid under a light microscope in the labs at Texas Biomed. The organoids have grown cilia, which are fine, hair-like structures that line the interior of the airway. Here, their movements appear like short flashes of light. A molecule is being moved along by the cilia, much like it would in the human body. Credit: Texas Biomed
Mucus created by a human airway organoid is moving in a clockwise direction as seen through a light microscope. The mucus is moved along with the help of cilia, which are fine, hair-like structures lining the airway. Credit: Texas Biomed
Papers:
Mostafa, A., Ye, C., Barre, R.S. et al. A live attenuated NS1-deficient vaccine candidate for cattle-origin influenza A (H5N1) clade 2.3.4.4.b viruses. npj Vaccines 10, 151 (2025). https://doi.org/10.1038/s41541-025-01207-9
Rothan, Hussin, Ahmed Mostafa, Mahmoud Bayoumi, Chengjin Ye, Ramya S. Barre, Anna Allué-Guardia, Aitor Nogales, Jordi B. Torrelles, and Luis Martinez-Sobrido. 2025. “Emerging Highly Pathogenic H5N1 Influenza Triggers Fibrotic Remodeling in Human Airway Organoids.” Emerging Microbes & Infections 14 (1). doi:10.1080/22221751.2025.2532684.