Many bladder cancer patients cannot tolerate the strong side effects of the gold standard treatment. Texas Biomed researchers have found a way to minimize those side effects and are poised to move into clinical trials with partners at UT Health San Antonio and Southwest Research Institute.
SAN ANTONIO (August 22, 2022) – A modified tuberculosis (TB) vaccine developed at Texas Biomed could help treat a form of bladder cancer, called non-muscle invasive bladder cancer, without strong side effects. Results in mouse models and human cells show promising results and pave the way for human clinical trials. The research, conducted in close collaboration with UT Health San Antonio, was published online in June in the journal Cancer Immunology, Immunotherapy.
“I’m hopeful that with grant or industry support, we can move this right along to clinical trials and explore this treatment for patients who don’t have options other than bladder removal,” says Robert S. Svatek, MD, a urologic oncologist who treats bladder cancer patients at the Mays Cancer Center at UT Health San Antonio and is co-senior author of the research paper.
Each year in the United States, about 61,700 men and 19,480 women get bladder cancer, and about 17,100 deaths due to the disease occur (12,120 men and 4,980 women), according to the American Cancer Society. Bladder cancer is the fourth most common type of cancer in men. About 75% of bladder cancer cases are classified as non-muscle invasive, which means the cancer affects the tissue lining the inner surface of the bladder, but not the bladder muscle.
The Mycobacterium bovis bacille Calmette-Guérin (BCG) vaccine was developed for tuberculosis in the 1920s, and has also been used to treat non-muscle invasive bladder cancer since the late 1970s by stimulating an immune response at the cancer site. It was one of the first cancer immunotherapies and is more effective than chemotherapy for this type of cancer – but up to 84% of patients cannot tolerate the strong side effects and don’t complete the three years of BCG treatment. When treatments fail, the last option is to remove the bladder, which leads to reduced quality of life.
“Imagine that there’s this great drug that works really well, but you’re not able to tolerate it,” Dr. Svatek says. “We’re talking about a very select group of patients, but for whom this really, really matters.”
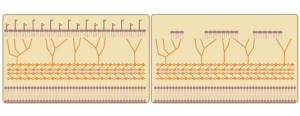
Texas Biomed Professor Jordi B. Torrelles, PhD, specializes in tuberculosis, and has been working on a modified BCG vaccine for the past six years to improve TB treatment in the lungs. Specifically, Dr. Torrelles and his team remove certain lipids from the cell envelopes of the bacteria in the BCG vaccine. This “delipidated” vaccine still triggers the body to produce well-regulated immune responses, but reduces overzealous inflammation that causes severe tissue damage.
“It is more targeted and allows for a longer, slower response, which makes it more effective,” Dr. Torrelles says.
Thanks to a San Antonio Medical Foundation grant, Dr. Torrelles was able to team up with Dr. Svatek and Hong Dixon, PhD, a research scientist specializing in drug development at Southwest Research Institute (SwRI), to test the modified vaccine for bladder cancer as well.
Dr. Torrelles and his lab made two versions of the delipidated vaccine based on different TB bacteria strains: one known as sub-strain TICE, which is developed in the U.S., and one known as sub-strain Tokyo, which is developed in Japan.
Dr. Svatek’s lab conducted the tests in a mouse model of bladder cancer and in cells collected from human cancer patients. They tested both delipidated BCG versions, and found that both were equally effective compared with the original BCG vaccine at killing the cancer, but that the modified Tokyo version performed better than the TICE version, with far less inflammation and minimal side effects.
“We were not expecting such a clear difference between the strains,” says Dr. Torrelles, who has patented the modified vaccine for bladder cancer. Now, the collaborators plan to seek funding for a phase 1 clinical trial in human patients. SwRI is assessing manufacturing the modified vaccine for the clinical trial.
“We are excited to see this move forward and since it is based on an already U.S. FDA-approved treatment, we are hopeful it can proceed in a timely way,” Dr. Torrelles says.
###
This is a joint release from Texas Biomedical Research Institute and The Mays Cancer Center at UT Health San Antonio.
Texas Biomed is one of the world’s leading independent biomedical research institutions dedicated to eradicating infection and advancing health worldwide through innovative biomedical research. Texas Biomed partners with researchers and institutions around the world to develop vaccines and therapeutics against viral pathogens causing AIDS, hepatitis, hemorrhagic fever, tuberculosis and parasitic diseases responsible for malaria and schistosomiasis disease. The Institute has programs in host-pathogen interactions, disease intervention and prevention, and population health to understand the links between infectious diseases and other diseases such as aging, cardiovascular disease, diabetes and obesity. For more information, go to www.TxBiomed.org.
The Mays Cancer Center at UT Health San Antonio is one of only four National Cancer Institute-designated Cancer Centers in Texas. The Mays Cancer Center provides leading-edge cancer care, propels innovative cancer research and educates the next generation of leaders to end cancer in South Texas. Visit www.Cancer.uthscsa.edu. Stay connected with The University of Texas Health Science Center at San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.